Fertility Preservation: Planning for the Future
May 12, 2025, 8:17 a.m.
Fertility preservation is a crucial option for individuals who wish to have children in the future but face circumstances that might affect their fertility. This article explores the reasons for fertility preservation, the available methods, success rates, and personal experiences to help you make informed decisions.
Many people choose fertility preservation for medical reasons. For instance, cancer treatments like chemotherapy and radiation can damage reproductive cells, leading to infertility. According to the American Cancer Society, certain cancers and their treatments can affect fertility in both men and women [source: American Cancer Society]. Other medical conditions, such as autoimmune diseases or genetic disorders, might also necessitate fertility preservation.
On the personal side, some individuals opt for fertility preservation to delay parenthood. This could be due to focusing on career, not having found the right partner, or simply wanting to have children later in life. With advancements in reproductive technology, it's now possible to preserve fertility for future use.

For Women: - Egg Freezing (Oocyte Cryopreservation): This involves stimulating the ovaries with fertility drugs to produce multiple eggs, which are then retrieved and frozen for future use. - Embryo Freezing: Similar to egg freezing, but the eggs are fertilized with sperm to create embryos before freezing. This requires a sperm donor or partner. - Ovarian Tissue Freezing: An experimental method where ovarian tissue is removed and frozen for later transplantation.
For Men: - Sperm Freezing (Sperm Cryopreservation): Sperm is collected and frozen for future use in assisted reproductive techniques. - Testicular Tissue Freezing: An experimental method for men who cannot produce sperm, involving freezing testicular tissue for future use.
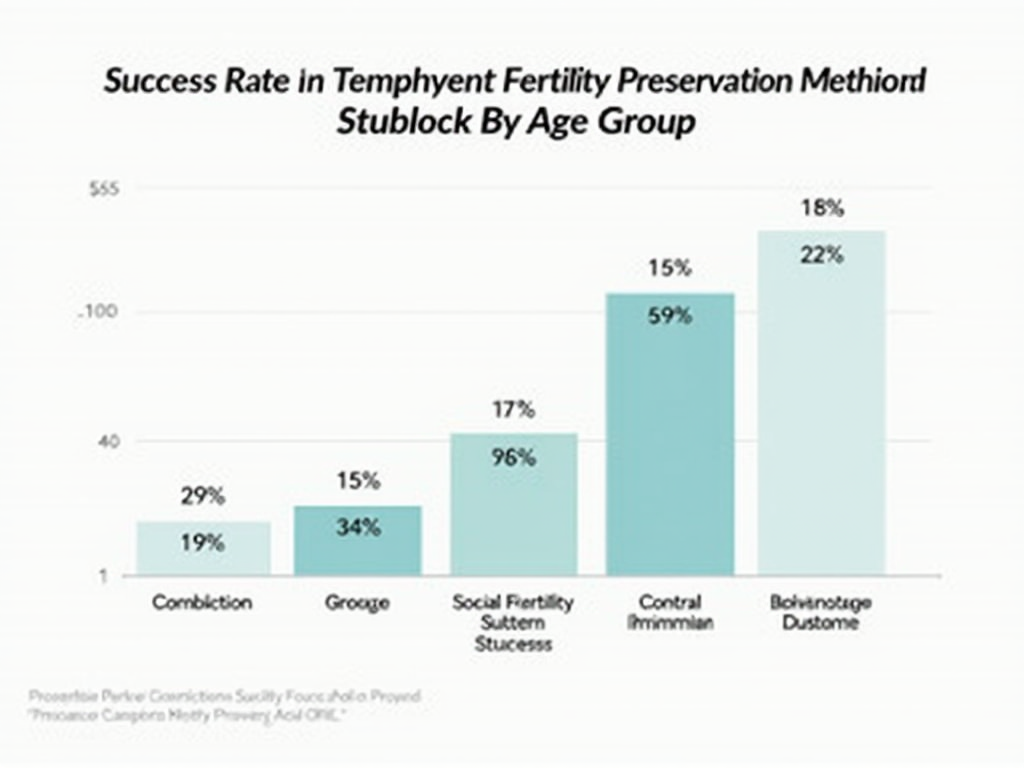
These methods have varying success rates and are chosen based on individual circumstances, age, and health conditions.

Fertility drugs are medications used to stimulate the ovaries to produce multiple eggs. In fertility preservation, they are often used in egg or embryo freezing procedures. Common fertility drugs include Clomiphene Citrate, Gonadotropins, and GnRH Agonists.
The success rates of fertility drugs vary. For example, Gonadotropins can lead to the retrieval of multiple eggs, increasing the chances of successful preservation. However, they also carry risks like ovarian hyperstimulation syndrome (OHSS). It's essential to discuss these risks with a healthcare provider.
The success of fertility preservation depends on several factors, including age, the method used, and the quality of the preserved cells or tissues. For egg freezing, the American Society for Reproductive Medicine reports that the chance of a live birth from frozen eggs is around 30-60% per embryo transfer, depending on the woman's age at the time of freezing [source: ASRM].
Real-life examples show varied outcomes. For instance, a woman who froze her eggs at 30 might have a higher success rate than someone who did so at 40. It's crucial to have realistic expectations and understand that fertility preservation is not a guarantee but an option.
Many individuals who have undergone fertility preservation share that the process can be emotionally challenging but ultimately empowering. For example, Sarah, a cancer survivor, chose to freeze her eggs before chemotherapy. She says, "It gave me hope for the future during a difficult time."
Others, like John, who froze his sperm before a vasectomy, appreciate the peace of mind it provides. "I might want kids later, and this ensures I have the option," he explains.
It's important to consider the emotional and psychological aspects, as the process can be stressful. Support from family, friends, or counseling can be beneficial.
Fertility preservation can be expensive, with costs varying widely depending on the method and location. For example, egg freezing can cost between $10,000 and $15,000 per cycle in the United States, not including storage fees [source: FertilityIQ].
Insurance coverage for fertility preservation is limited and varies by provider and location. Some employers offer fertility benefits, so it's worth checking with your HR department.
Legally, there are considerations regarding the ownership and use of preserved genetic material, especially in cases of divorce or death. It's advisable to consult with a lawyer specializing in reproductive law.
Long-term storage of preserved cells or tissues requires ongoing fees and planning. Most clinics offer storage for up to 10 years, with options to extend.

Fertility preservation offers hope and options for those facing medical treatments or personal circumstances that might affect their fertility. By understanding the methods, success rates, and personal experiences, individuals can make informed decisions about their reproductive future.
It's essential to consult with healthcare providers, consider the financial and legal aspects, and seek support throughout the process. While not a guarantee, fertility preservation is a valuable tool for planning for the future.
Research is ongoing in the field of fertility preservation, with new technologies being developed. For example, in vitro maturation (IVM) allows immature eggs to be collected and matured in the lab before freezing, which can be beneficial for women who cannot undergo ovarian stimulation.
Another area of research is the use of artificial intelligence to select the best eggs or embryos for freezing, potentially improving success rates.
While these technologies are promising, they are still in the experimental stages and not widely available. It's important to stay informed about advancements in the field.