Latest Advances in Assisted Reproductive Technology: Breaking Barriers in Fertility Treatment
April 29, 2025, 8:05 a.m.
Overview
Assisted reproductive technology (ART) has transformed the landscape of fertility treatment, offering hope to millions struggling with infertility. From in vitro fertilization (IVF) to genetic screening, ART encompasses a range of procedures designed to assist in conception. Recent advances are pushing the boundaries even further, improving success rates and expanding possibilities for prospective parents. This article delves into the latest breakthroughs in ART, exploring how they work, their benefits, and what they mean for the future of reproductive medicine.

Artificial Intelligence in Embryo Selection
One of the most exciting developments in ART is the use of artificial intelligence (AI) to select the best embryos for implantation. Traditionally, embryologists rely on visual inspection to choose embryos based on morphology. However, this method can be subjective and may not always predict success accurately.
AI algorithms, trained on vast datasets of embryo images and outcomes, can analyze subtle features that might be invisible to the human eye. By assessing factors like cell division rates and symmetry, AI can predict which embryos are most likely to lead to a successful pregnancy. This not only improves the chances of conception but also reduces the time and emotional toll on patients by minimizing the number of IVF cycles needed.
For example, a study published in the journal Nature Medicine found that an AI system could predict embryo viability with over 90% accuracy, significantly higher than traditional methods. [Link to study: "AI in embryo selection" - https://www.nature.com/articles/s41591-020-01187-9]

Mitochondrial Replacement Therapy: Preventing Genetic Diseases
Mitochondrial replacement therapy (MRT) is a groundbreaking technique aimed at preventing the transmission of mitochondrial diseases from mother to child. Mitochondrial diseases are caused by defective mitochondria, which are inherited solely from the mother.
In MRT, the nucleus of the mother's egg is transferred to a donor egg with healthy mitochondria, which is then fertilized with the father's sperm. This results in an embryo with nuclear DNA from both parents and mitochondrial DNA from the donor, effectively eliminating the risk of mitochondrial disease.
While still in its early stages and subject to ethical debates, MRT has shown promise in clinical trials. In 2016, the first baby was born using this technique, marking a significant milestone in reproductive medicine. [Link to news article: "First baby born using mitochondrial replacement therapy" - https://www.newscientist.com/article/2107219-first-baby-born-using-3-parent-technique-to-treat-infertility/]

Ovarian Tissue Cryopreservation: Preserving Fertility for the Future
For individuals facing medical treatments that may compromise their fertility, such as chemotherapy, ovarian tissue cryopreservation offers a way to preserve their reproductive potential. This technique involves removing and freezing ovarian tissue before treatment, which can later be transplanted back to restore fertility.
Recent advances have improved the success rates of this procedure. For instance, refinements in freezing techniques and transplantation methods have led to more live births from cryopreserved ovarian tissue. According to the American Society for Reproductive Medicine, over 130 live births have been reported worldwide using this method as of 2020. [Link to ASRM: "Ovarian tissue cryopreservation" - https://www.asrm.org/topics/topics-index/ovarian-tissue-cryopreservation/]

In Vitro Gametogenesis: Creating Gametes from Stem Cells
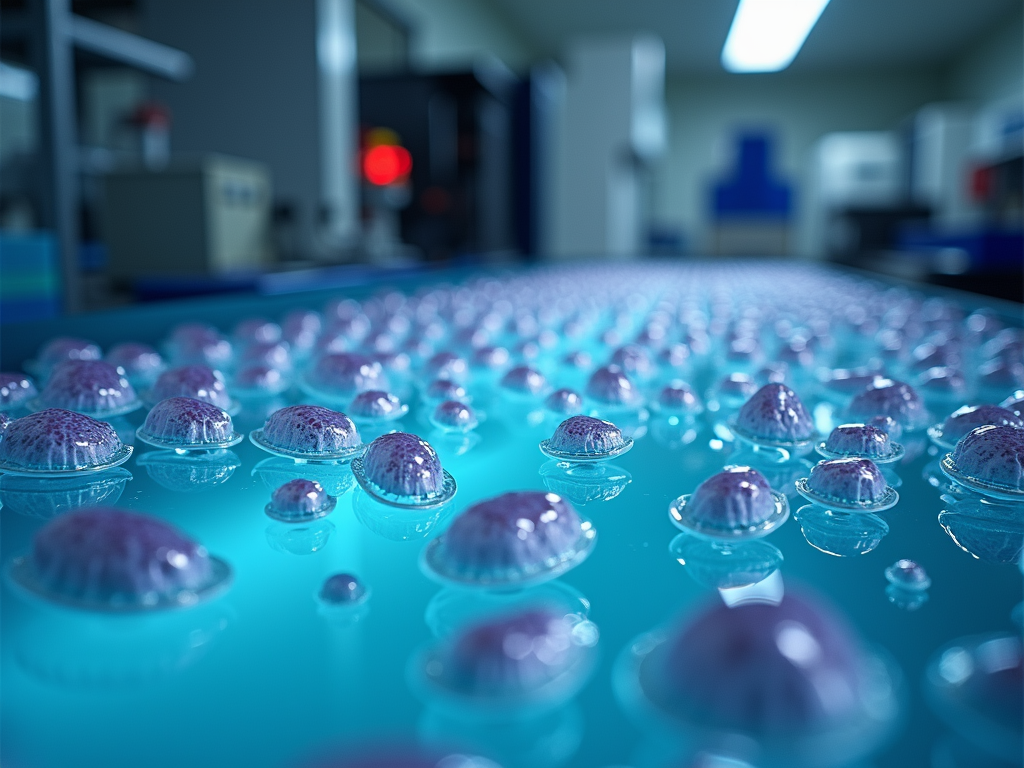
In vitro gametogenesis (IVG) is an emerging technology that aims to create eggs and sperm from stem cells. This could revolutionize fertility treatment by providing gametes for individuals who cannot produce them naturally, such as those with certain genetic conditions or who have undergone gonadotoxic therapies.
While still largely experimental, IVG has been successfully demonstrated in animal models, and researchers are working towards translating this to human applications. The potential of IVG extends beyond fertility treatment; it could also enable same-sex couples to have biological children together.
However, IVG raises complex ethical and safety concerns that need to be addressed before it can be widely adopted. [Link to review article: "In vitro gametogenesis: ethical considerations" - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7325787/]
Personalized Fertility Treatments: Tailoring Care with Genetics
Advances in genetic profiling are enabling more personalized approaches to fertility treatment. By analyzing an individual's genetic makeup, clinicians can identify specific factors that may affect fertility and tailor treatments accordingly.
For example, genetic tests can reveal mutations that impact ovarian reserve or response to fertility drugs, allowing for customized medication protocols. Additionally, preimplantation genetic testing (PGT) can screen embryos for chromosomal abnormalities before implantation, increasing the likelihood of a healthy pregnancy.
A study in the Journal of Assisted Reproduction and Genetics highlighted how personalized treatment plans based on genetic data improved IVF success rates by up to 20%. [Link to study: "Personalized medicine in ART" - https://link.springer.com/article/10.1007/s10815-019-01587-2]

Fertility Drugs and Age Factors: Navigating the Challenges
Fertility drugs play a crucial role in ART by stimulating ovulation and enhancing the chances of conception. Common medications include clomiphene citrate, gonadotropins, and aromatase inhibitors. However, their effectiveness can be influenced by age, as fertility naturally declines with advancing maternal age.
Women over 35 may have a reduced ovarian reserve, meaning fewer eggs are available for stimulation. Consequently, they might require higher doses of fertility drugs or different protocols to achieve optimal results. Understanding these age-related factors is essential for setting realistic expectations and choosing the most appropriate treatment plan.
For instance, a meta-analysis in the Fertility and Sterility journal found that women over 40 had significantly lower live birth rates with IVF compared to younger women, even with the use of fertility drugs. [Link to meta-analysis: "Age and IVF outcomes" - https://www.fertstert.org/article/S0015-0282(17)31938-4/fulltext]

Conclusion
The field of assisted reproductive technology is advancing at a remarkable pace, offering new hope and possibilities for individuals and couples facing infertility. From AI-driven embryo selection to genetic innovations and personalized treatments, these breakthroughs are not only improving success rates but also making fertility care more accessible and tailored to individual needs. As research continues, we can expect even more exciting developments that will further transform the landscape of reproductive medicine.