How to Diagnose Infertility in Women: A Comprehensive Guide
May 1, 2025, 5:25 p.m.
Infertility is a challenging issue that affects many women around the world. If you're struggling to conceive, understanding how infertility is diagnosed can help you navigate this complex journey. This guide will walk you through the step-by-step process of diagnosing infertility in women, from initial doctor visits to specialized tests, while also addressing the emotional toll it can take.

What is Infertility?
Infertility is defined as the inability to conceive after one year of regular, unprotected intercourse. For women over 35, this period is shortened to six months. According to the Centers for Disease Control and Prevention, about 10% of women in the United States have difficulty getting pregnant or staying pregnant. Infertility can be caused by a variety of factors, including ovulation disorders, blocked fallopian tubes, uterine abnormalities, or age-related decline in fertility.
When to Seek Help for Infertility
If you're under 35 and have been trying to conceive for a year without success, it's time to consult a doctor. For women over 35, it's recommended to seek help after six months of trying, as fertility declines with age. Additionally, if you have irregular menstrual cycles, a history of pelvic infections, or other known reproductive issues, you should see a doctor sooner.
Initial Steps in Diagnosis
The journey to diagnose infertility typically begins with a visit to a healthcare provider, often a gynecologist or a fertility specialist. During this initial consultation, the doctor will ask about your medical history, including:
- Menstrual cycle regularity
- Previous pregnancies or miscarriages
- Surgeries or medical conditions
- Medications you're taking
- Lifestyle factors such as smoking, alcohol use, or stress levels
This conversation helps the doctor identify potential causes of infertility and determine which tests to order next.
It's important to be open and honest during this discussion. Many women feel embarrassed or uncomfortable talking about their reproductive health, but remember that your doctor is there to help. Providing accurate information can lead to a more accurate diagnosis.
Physical Examinations
After reviewing your medical history, the doctor will likely perform a physical examination. This may include:
- A general physical exam to check for any signs of hormonal imbalances, such as excess hair growth or acne.
- A pelvic exam to inspect the reproductive organs for abnormalities like fibroids or cysts.
These exams are usually quick and non-invasive, but they provide valuable information about your overall health and reproductive function.
In some cases, the doctor might also measure your body mass index (BMI), as being underweight or overweight can affect fertility. If any issues are detected during the physical exam, further tests may be recommended.

Laboratory Tests
Laboratory tests are a crucial part of diagnosing infertility. These tests help assess hormone levels, ovarian function, and other factors that can affect fertility. Common laboratory tests include:
- Follicle-Stimulating Hormone (FSH): Measured on day 3 of the menstrual cycle, FSH levels can indicate ovarian reserve.
- Luteinizing Hormone (LH): Also measured on day 3, LH helps assess ovulation.
- Estradiol: This hormone is checked alongside FSH to evaluate ovarian function.
- Progesterone: Measured about a week after ovulation to confirm that ovulation occurred.
- Thyroid Hormones: Thyroid disorders can impact fertility, so TSH and other thyroid hormones may be tested.
- Prolactin: High levels of prolactin can interfere with ovulation.
Additionally, tests for sexually transmitted infections (STIs) might be conducted, as some STIs can cause infertility.
One important test is the Anti-Mullerian Hormone (AMH) test, which provides an estimate of the number of eggs remaining in the ovaries. A low AMH level may suggest diminished ovarian reserve, while a high level could indicate conditions like polycystic ovary syndrome (PCOS). For more information on AMH testing, you can refer to the American Society for Reproductive Medicine's guide.

Imaging Studies
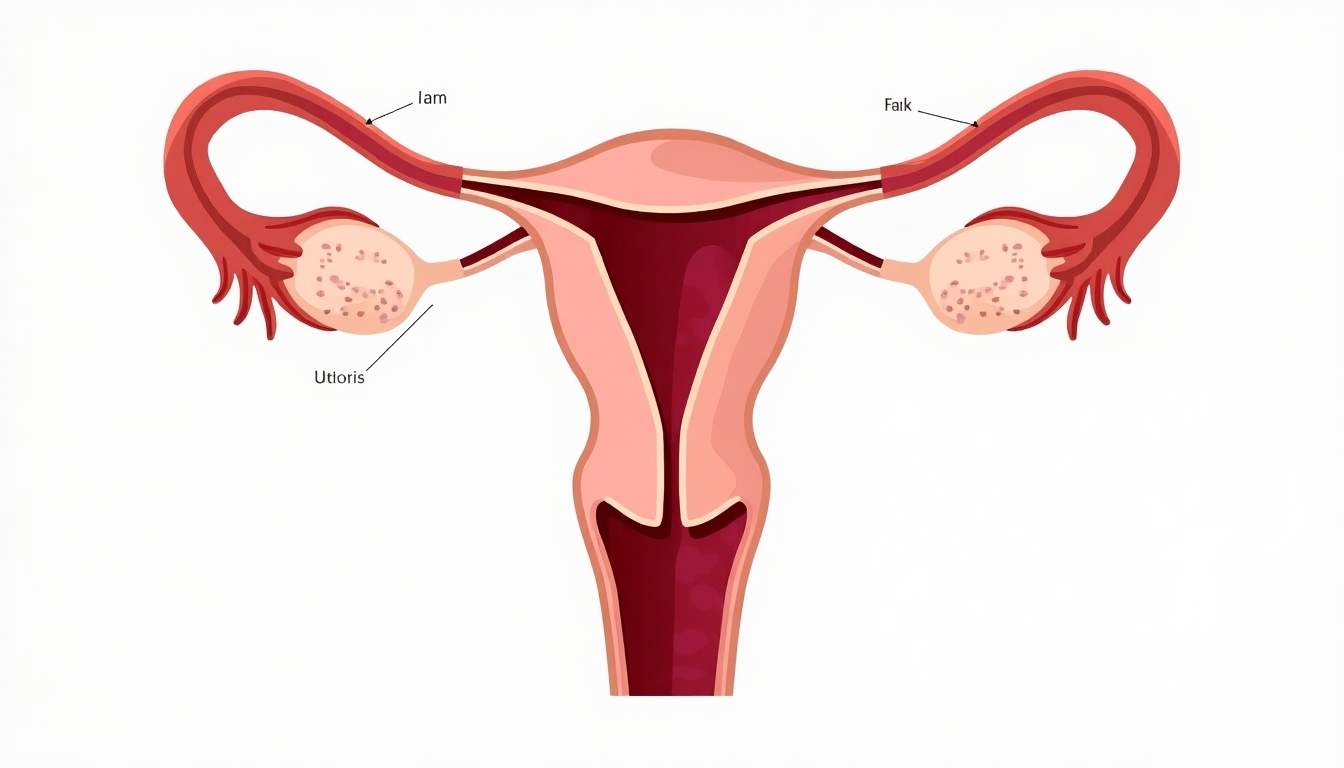
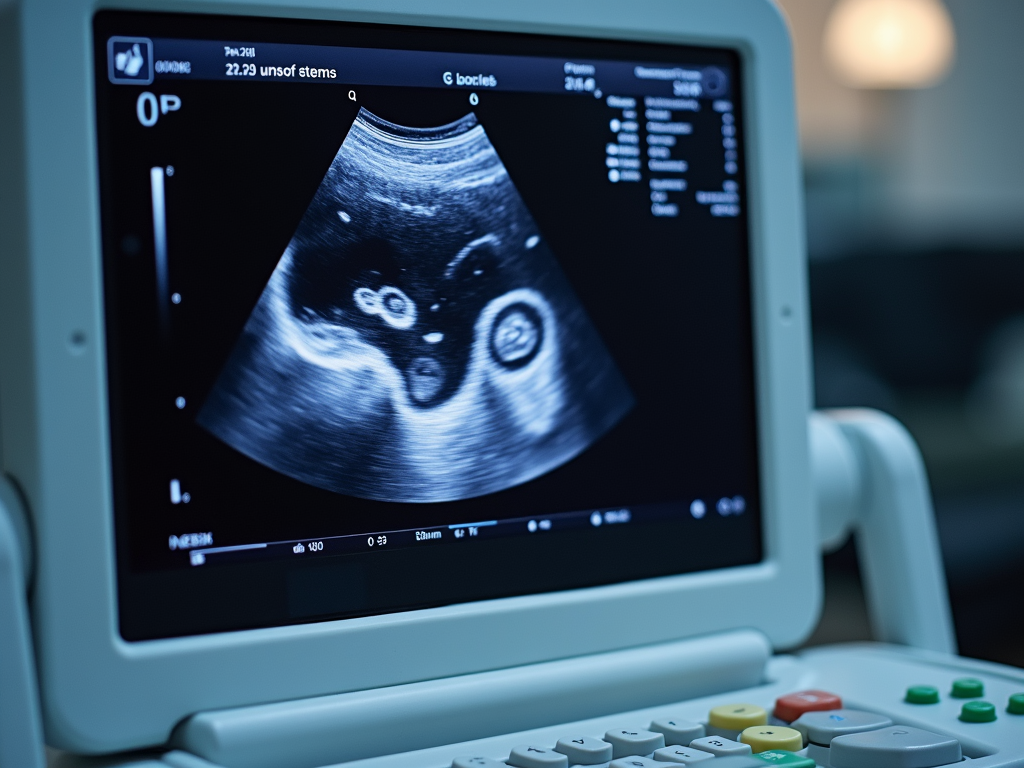
Imaging studies allow doctors to visualize the reproductive organs and identify any structural abnormalities. The most common imaging test is the transvaginal ultrasound, which uses sound waves to create images of the ovaries and uterus. This can help detect issues like ovarian cysts, uterine fibroids, or polyps.
Another important test is hysterosalpingography (HSG), where a dye is injected into the uterus, and X-rays are taken to check if the fallopian tubes are open. Blocked fallopian tubes are a common cause of infertility.
During an HSG, you might feel some discomfort or cramping, but the procedure is usually quick. It's important to discuss any concerns with your doctor beforehand.
Specialized Procedures
In some cases, more invasive procedures may be necessary to diagnose infertility. These include:
- Laparoscopy: A surgical procedure where a small camera is inserted through an incision in the abdomen to look for endometriosis, pelvic adhesions, or other issues.
- Hysteroscopy: A procedure where a thin scope is inserted into the uterus to examine the uterine cavity for abnormalities like polyps or fibroids.
These procedures are typically done under anesthesia and may require a short recovery period.
While these procedures carry some risks, they can provide definitive diagnoses and sometimes even treat the underlying issue during the same procedure.

Emotional and Psychological Aspects
Going through the process of diagnosing infertility can be emotionally taxing. Many women experience feelings of anxiety, sadness, or frustration as they navigate the various tests and procedures. It's important to acknowledge these feelings and seek support when needed.
Consider joining a support group for women dealing with infertility, or talking to a counselor who specializes in reproductive issues. Remember that you're not alone, and there are resources available to help you cope. The Resolve: The National Infertility Association offers valuable resources and support.

Summary
Diagnosing infertility in women involves a series of steps, starting with a thorough medical history and physical examination, followed by laboratory tests, imaging studies, and possibly specialized procedures. While the process can be daunting, understanding what to expect can help you feel more prepared and in control. If you're facing infertility, know that there are many treatment options available, including in vitro fertilization (IVF), and support systems to help you through this journey.