The Role of IVF in Modern Reproductive Medicine
May 3, 2025, 7:28 a.m.
Overview
In vitro fertilization (IVF) has transformed reproductive medicine, giving hope to couples struggling with infertility, including male infertility issues like oligospermia. This article dives into the role of IVF in modern healthcare, its process, success rates, and its broader impact.
What is IVF?
IVF, or in vitro fertilization, is a process where doctors combine an egg and sperm outside the body to help people have a baby. It’s a key part of modern reproductive medicine, assisting those who can’t conceive naturally. The journey began in 1978 with Louise Brown, the first IVF baby. Since then, millions of children have been born this way.
IVF tackles many fertility problems. For women, it helps with blocked tubes or irregular ovulation. For men, it addresses issues like oligospermia, a condition where sperm count is low. This flexibility makes IVF a go-to solution for infertility today.

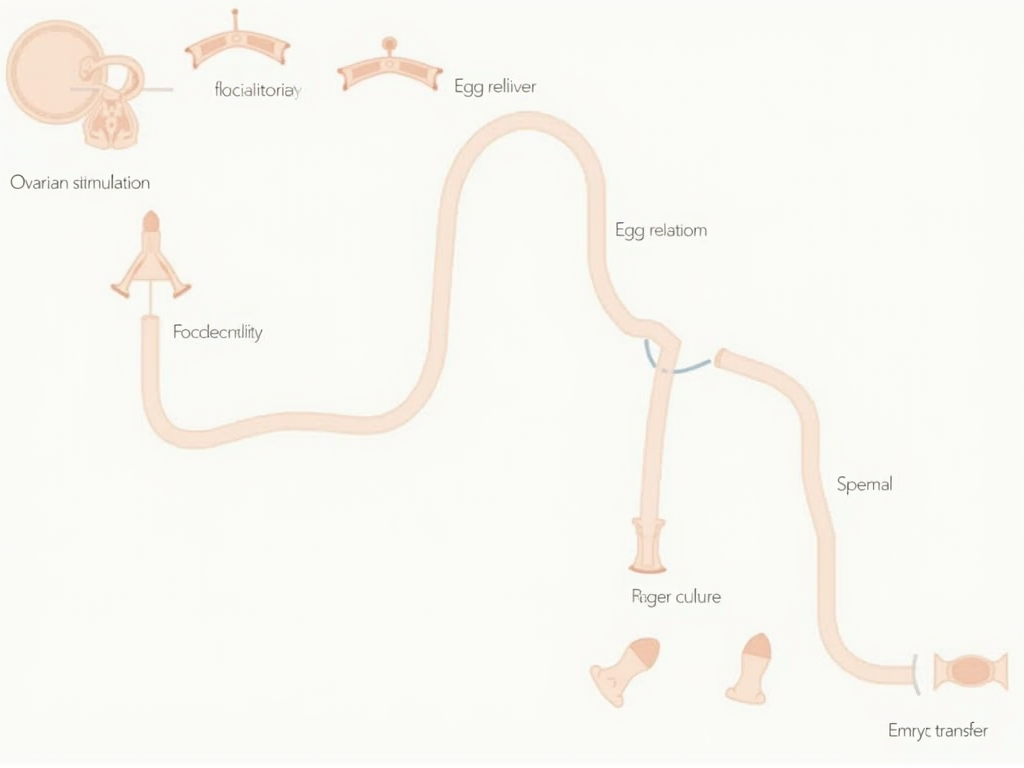
How IVF Works
The IVF process involves several clear steps. First, women take medicines to boost egg production. Doctors then retrieve those eggs with a simple procedure. Meanwhile, men provide a sperm sample—or sometimes donor sperm is used.
Next, the lab combines eggs and sperm. If sperm quality is poor due to oligospermia, a technique called ICSI injects a single sperm into an egg. After a few days, healthy embryos are placed in the woman’s uterus to grow.
IVF and Infertility
Infertility affects about 1 in 8 couples in the U.S., according to the CDC. Causes vary—hormone issues, age, or lifestyle factors. IVF steps in as a powerful tool, offering a chance at parenthood when other methods fail.
For many, infertility feels overwhelming. IVF doesn’t just treat physical barriers; it restores hope. Statistics show over 8 million babies have been born via IVF worldwide since it started, proving its impact in modern medicine.
Male Infertility and Oligospermia
Male infertility often stems from oligospermia, where a man has fewer sperm than normal. Doctors diagnose it with a simple test. If sperm count is low, natural conception becomes tough—but IVF changes that.
In cases of oligospermia and assisted reproductive technologies like IVF, success rises. ICSI, paired with IVF, targets the healthiest sperm, boosting the odds. This makes IVF a lifeline for men facing infertility challenges.

The IVF Journey
Starting IVF can feel like a rollercoaster. Couples often face stress, excitement, and uncertainty. One person might say, ‘It’s tough, but seeing our baby made every moment worth it.’ Emotional support from partners or counselors helps a lot.
Money matters too. IVF costs around $12,000 per cycle in the U.S., and insurance doesn’t always cover it. Some save up, while others explore financing. Knowing your options makes the journey smoother.

Success Rates and Factors
IVF success depends on age and health. Here’s a quick look:
| Age Group | Success Rate |
|---|---|
| Under 35 | 40-50% |
| 35-37 | 30-40% |
| 38-40 | 20-30% |
| Over 40 | 10-20% |
Younger women see better results, but lifestyle and clinic quality play roles too.
Want to improve your chances? Quit smoking, eat well, and pick a trusted clinic. Ask your doctor about success rates—they’ll give you a realistic picture based on your situation.

Ethical Considerations and Future Directions
IVF raises big questions. Should parents choose embryo traits? What about unused embryos? These debates shape laws and clinic rules. Experts like those at the American Society for Reproductive Medicine guide the conversation.
Looking ahead, IVF keeps advancing. New tools like genetic testing or better freezing methods improve outcomes. Some even dream of artificial wombs, though that’s years away. The role of IVF in modern reproductive medicine only grows stronger.

Summary
IVF has reshaped reproductive medicine, tackling infertility—including male infertility like oligospermia—with remarkable success. It’s a blend of science and hope, evolving to help more people build families. As technology advances, IVF’s impact will keep expanding.